Hello, SuperCaptainBraveFAM!
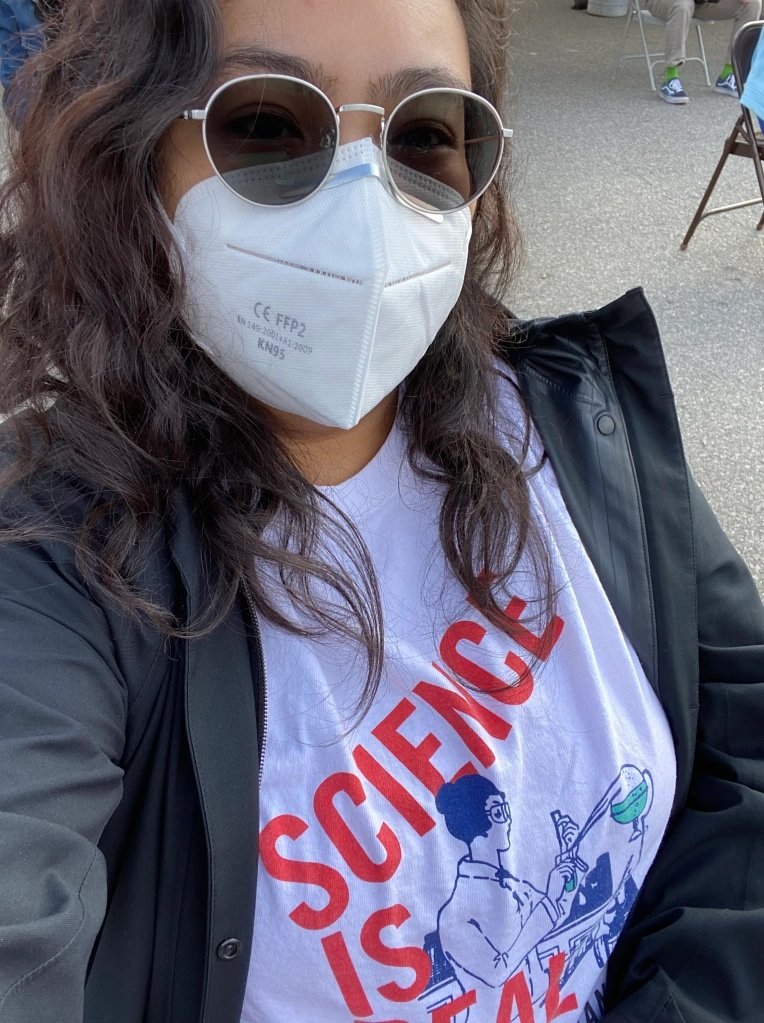
If you are a new reader to the blog, welcome! I’m Nurse Leah. I am a Licensed Vocational Nurse and work in the home healthcare sector.
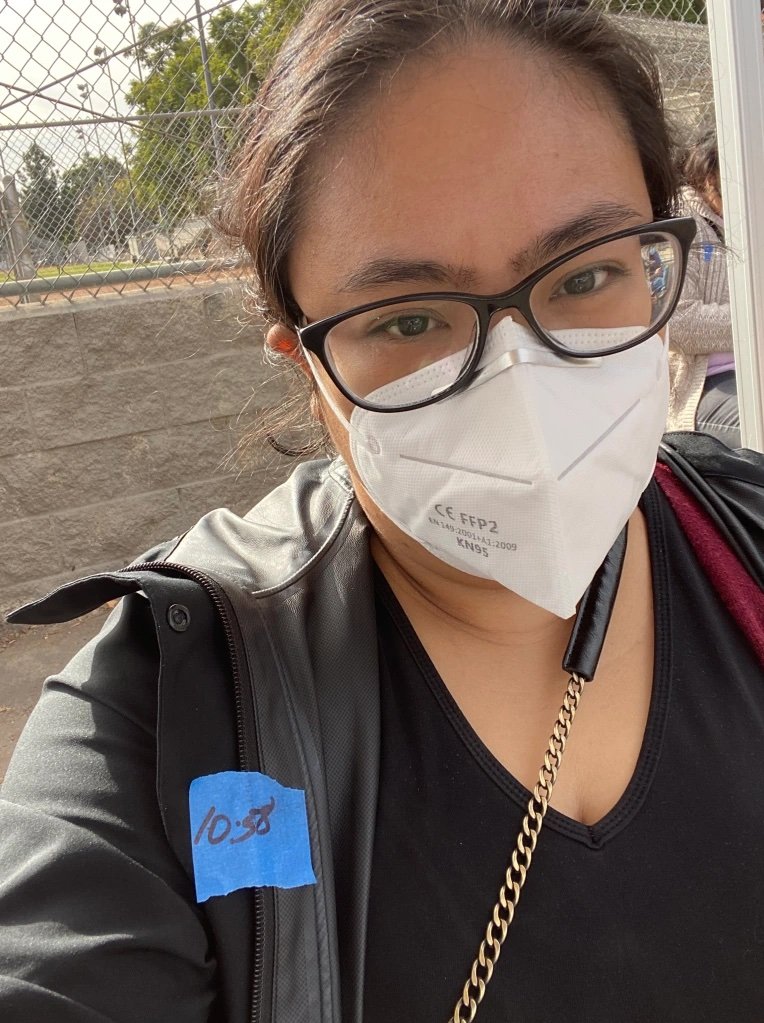
Which—at the time of writing—puts me in the Phase 1A, Tier 2 group of the LA County Vaccine Distribution Plan and makes me eligible to receive the Pfizer or Moderna vaccines for COVID-19.
I received the first dose of the Moderna vaccine for COVID-19 on January 7, with the second dose scheduled 28 days later. Which happens to be today, February 4.
Today, I’m going to go over what I know and have found out about how both the Moderna & Pfizer vaccines work and commonly asked questions about the vaccines. In Part 2, I’ll talk about my own journey with signing up, receiving, and side effects I experienced with regards to the injections.
Right off, I have to admit that I am firmly pro-vaccine. The science behind vaccines is sound and makes sense to me. I totally understand why certain people are vaccine hesitant or want to wait before allowing their kids to get this vaccine. (More on the reasons why in a bit.) But overall, the scientific approach toward vaccines in general, and for the COVID-19 vaccines in particular, is one that I have trust in.
I will put links for the info I have at the bottom of the blog. I’ll also try my best to use mostly casual knowledge that I have about immunology from my pre-nursing days to keep the blog from getting too technical.
So, buckle up, cuz ahead thar be science.
~Nurse Leah
How do vaccines work?
If I’m remembering my AP Bio correctly, then vaccines work by priming or “jump starting” the body’s immune response to the presence of a specific pathogen. The pathogen could be a virus or bacteria that causes you to get sick. Your immune system is in place to identify and destroy these body invaders.
There are special proteins on the surface of practically every cell ever. And every type of cell can have a different sequence of these proteins. Think of them like calling cards, keys, or (in my attempt to connect with today’s youth) hashtags. Each one is unique to that pathogen and one of the jobs of the immune system is to keep track of these “hashtags” and prevent certain ones from flooding the body’s newsfeed.
When you get a vaccine, it’s giving your immune system an example of the pathogen. Your immune system then creates antibodies that identify that pathogen and signals the need to fight/destroy/ban the identified cell from your body.
So, when the actual pathogen shows up, your immune system recognizes and can destroy it before it can spread and make you sick.
One question that my mom asked when I told her I got the vaccine was “Do you have COVID-19 now?”
In one word my answer was: no.
And allow me to explain why.
There are different types of vaccines and a lot of that has to do with how well they work at priming our immune system for fighting and keeping the body from getting the disease. One of the most common types of vaccines are live-attenuated vaccines. This is where a live, weaker version of the pathogen is introduced into your body for your immune system to identify and remember.
If you guys are curious about the different types of vaccines, leave a comment down below and I can rev up my research machine and write about that in the future.
There are other companies working on vaccines as well. Just because Pfizer and Moderna received permission to distribute their vaccines first doesn’t mean they’re the GOAT (Greatest of All Time) at protecting us against getting COVID-19.
However, both the Pfizer and Moderna vaccines are mRNA vaccines. There is no live virus in the dose and those who receive it do not contract COVID-19 from the injection.
Now on to the question: What is mRNA?
It sounds like another science-y word. DNA. And you’d be right. But they’re not the same thing.
mRNA stands for messenger RiboNucleic Acid
(It’s not spelled that way. It’s just a way for me to visualize why it’s abbreviated the way it is.)
DNA stands for DeoxyriboNucleic Acid
They’re both nucleic acids. But do different things. And mRNA cannot change the DNA of a cell.
mRNA is used by all cells to help create proteins that the cell then uses for whatever job it’s coded for.
So, what does an mRNA vaccine do exactly?
Using techniques learned over decades, scientists were able to analyze and isolate a specific protein spike from the SARS-CoV2 virus. This is the virus that causes COVID-19. Once the sequence of the protein spike was determined, scientists then created an mRNA sequence that re-creates the SARS-CoV2 protein spike onto non-SARS-CoV2 cells.
When the body’s immune system interacts with body cells that have the SARS-CoV2 protein spike, an immune response occurs and antibodies are formed. Remember that antibodies are how the body recognizes and identifies pathogens.
The faster your immune system can recognize a pathogen like SARS-CoV2, the faster your immune system can mobilize to get rid of it.
Going back to the hashtag metaphor, your Immune System is like an admin for the social media group that is your Body.
The SARS-CoV2 virus is like one of those automated spam bot accounts that comment on everyone’s posts with scams. And in every comment it makes, it has the hashtag for COVID-19.
The current mRNA vaccines know what the COVID-19 hashtag looks like and reports it to the Immune System.
Now the Immune System can do its admin thing and delete/destroy/ban every comment with the hashtag for COVID-19.
And in the end, it leaves the Body’s newsfeed clear of the illness and clutter the SARS-CoV2 spam bot left behind.
Is the vaccine safe?
Every drug and modern technique used in medicine has a balance of risks and benefits. What types you use and feel safe using should be discussed fully and honestly with your doctor. Remember that they are on your side and if you have any concerns, you have the right to voice them and ask for further clarification on any aspect of your care.
When the FDA gave Emergency Use Authorizations to the Moderna and Pfizer vaccines, there was a whole process involved where scientists and physicians went over the collected data supplied by the companies and weighed the benefits versus the risks of allowing the use of the vaccines.
You can find a quick infographic of the process here. As of January 31, 2021, some news outlets report that a third vaccine—this one produced by Johnson & Johnson—is expected to apply for an Emergency Use Authorization for their COVID-19 vaccination in early February.
The vaccines offered by Moderna and Pfizer are as safe as they can be given the facts and processes the scientific studies have shown at this time.
It sounds like a non-answer. Believe me, typing that was somewhat difficult for me.
But it’s also the truth.
And it’s a lot better than hearing the words “We’ll see” from your parents when you ask for that toy that's just this shy of dangerous.
What are the Side Effects?
As mentioned before, there are risks and benefits to any medication.
Common side effects that both the Moderna and Pfizer vaccines share are:
At the injection site:
General side effects:
The serious side effects are along the lines of a severe allergic reaction. Which include difficulty breathing, swelling of the face and throat, a fast heartbeat, a bad rash all over the body, and dizziness & weakness. Severe allergic reactions like this are called anaphylaxis.
If you’re like me and have family members with shellfish allergies, it’s a very concerning issue when considering whether or not to get either vaccine.
If there is any chance that you believe an allergic reaction is possible for you or a loved one—for example, if the person getting the vaccine keeps an Epinephrine pen (Epi-Pen) with them at all times because of an already known allergy—then I strongly suggest talking to your doctor to create a personalized plan for when it is time to get the vaccine.
So…who can get the vaccine?
I mentioned earlier that the vaccines offered at the time of writing this blog were given Emergency Use Authorization by the FDA. After reviewing the information given to them by the companies, the FDA created guidelines on the use of each vaccine based on their knowledge of the safety and efficacy of the vaccine. (Efficacy means how well the vaccine does to prevent infection by the SARS-CoV2 virus.)
For the Pfizer vaccine, the FDA authorization allows those 16 years old and older to get the vaccine.
For the Moderna vaccine, the FDA authorization allows those 18 years old and older.
The reason for these particular ages has to do with the ages of the people involved in the clinical trials at each company. The data available only included people above the ages listed. It’s also because the data in the clinical trials is contained to the age group listed that the vaccines aren’t currently available for children.
There also isn’t a lot of data about the vaccine’s effect on pregnant or breastfeeding women. During the time of the clinical trials, there were several pregnancies reported after the start of the trials in the groups taking part, but at the time of writing, there is no information on any negative side effects in either mother or child in relation to the vaccine.
The only people in the allowed age range who absolutely should NOT get either COVID-19 vaccine are those who’ve had a severe allergic reaction to a previous dose of the vaccine or who’ve had a severe allergic reaction to any of the ingredients of the vaccine.
The documents of outlining the Emergency Use Authorizations of each vaccine are available to the public on the FDA website. If you want to read more about them, you can find the Moderna EUA Fact Sheet and the Pfizer EUA Fact Sheet by clicking the links.
When will the vaccine be available for children?
Walk down any medicine aisle in a grocery store and you’ll find a section with brightly colored boxes with the word CHILDREN’S splashed before the name of many familiar medications. It’s more than just an issue of changing the amounts and ratios for smaller humans. It’s about achieving the desired chemical reactions.
The way children’s bodies react to medicine can be different than adults. So separate studies and clinical trials for children of different ages need to happen before any vaccine can be available for kids. Any data for adjustments that might need to happen to make the vaccine just as effective for kids as in adults is collected during this period.
The way that Emergency Use Authorizations work in the case of vaccines is that the company must wait 60 days after 50% of the clinical trial group gets their last dose of the vaccine to apply for the authorization. This allows scientists and doctors time to check for any side effects. The process is the same for any clinical trial that includes adolescents and children.
In a January article in Bloomberg, it was reported that the Pfizer vaccine trial for adolescents ages 12-15 completed enrollment for volunteers. Which means the clinical trial with actual administered doses of vaccine should start soon.
In the same article, Moderna reported that the first doses in their vaccine trial for adolescents ages 12-18 were given in December. With the current timeline of the second dose given at 28 days after the first, it’s entirely possible for the Moderna vaccine to be eligible for an Emergency Use Authorization for children in that age range by the time the 2021-2022 school year starts.
There will be trials for younger kids, too. And those will go through the same process in order to get the Emergency Use Authorization from the FDA.
Which, being the mom of a current 4th grader, sounds ah-maze-ing. But, seeing as how my 4th grader has a high chance of having a shellfish allergy (we haven’t tested this theory yet), I’m still nervous.
With either company, the road to getting the vaccine into the arms of our kids is a long one. And given the current rollout in the U.S. for giving vaccines to the adults, patience is a virtue we’ll definitely need.
But what is it like getting the COVID-19 vaccine?
That is a great question. And one that honestly deserves its own blog post. Whatever you may feel about the current state of vaccine administration, I will share my own experience with the Moderna COVID-19 vaccine from finding out if I was eligible to receive it to the side effects I felt in the days after the shot. And with California making individuals 65 and over eligible as well, I can share what steps I took to make sure my mother got her vaccine safely and quickly.
Stay safe and stay brave, SuperCaptainBraveFAM!
"I Got the COVID-19 Vaccine: Part 2" is coming up on Monday, February 8th. So, don’t forget to subscribe to our mailing list, like, and follow us on social media for more content and upcoming announcements!
www.supercaptainbraveman.com
Instagram: @supercaptainbraveman
Facebook: www.facebook.com/supercaptainbraveman
For further information regarding COVID-19 and the vaccines mentioned in this blog, please visit:
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html
https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines
https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine#additional
https://www.fda.gov/vaccines-blood-biologics/vaccines/emergency-use-authorization-vaccines-explained
https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine
Congratulations for reading this far down the blog!
As an extra, here’s the link to a video made by one of my favorite science YouTube channels: ASAP Science. In it they talk about the effects of mRNA vaccines on the human body. Enjoy! https://youtu.be/the81FQoAUI